

|
|
|
|
|
|
THE ANATOMY OF THE PENIS
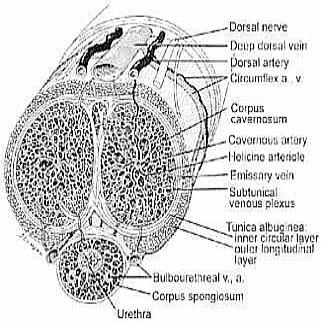
The anatomy of the penis is made up of three separate cylinders. The two paired cylinders called the corpora cavernosa make up the majority of the bulk and the erectile functioning of the penis. Both these cylinders actually communicate with each other for approximately three-quarters of their length through small holes between the cylinders. As the penis approaches the body, these two cylinders split and are anchored to the pelvic bone by a tough membrane. Each of these cylinders is encased in a very tough thick sheath called the tunica albuginea. A tough thick membrane surrounds the penis so that when it is filled with blood under pressure it creates a firm structure that allows penetration. The third cylinder of the penis is called the corpus spongiosum, and it contains the urethra. The tissue around this erectile body is much thinner, and the cylinder actually sits in a groove created by the other two cylinders. As this structure approaches the end of the penis, it becomes swollen and is known as the glans, or the head of the penis. As this layer gets closer to the body, it expands to form the bulb. Covering all three of these cylinders is a thick tough membrane called Buck's fascia. Finally, a final layer covers this area called Colles fascia, or the superficial layer. This is actually continuous with the abdominal wall and makes this whole supporting structure of the penis very tough, allowing it to take quite a bit of force and trauma.
The skin covering the penis is extremely mobile and expandable. This is necessary to allow an erection to take place. The skin of the penis is unique in this property, and it is controlled by the hormonal system. The head of the penis, or the glans, is an anatomically distinct structure covered by a foreskin. This is a double layer of penile skin that is very freely moveable. The body of the penis is anchored to the pubic bone, and a thickening of the rectus muscle anchors the top of the penis. The rectus muscles, are the muscles in the middle of the abdominal wall. This thickened layer, called the fundiform ligament, extends off the rectus muscle to anchor the penis. When this ligament is cut, as in so-called penis-lengthening operations, the penis may appear longer although it simply hangs lower from the body because it is disattached.
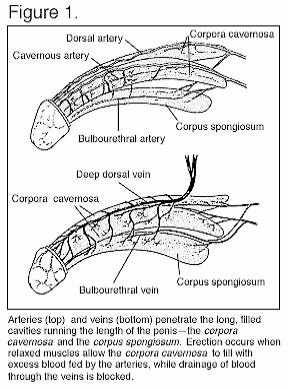
Blood Supply
The blood supply of the penis comes from a main blood vessel that goes down the back of the body called the aorta. The aorta then branches to an internal and external iliac artery, and finally a pudendal artery passes underneath the pelvic bone and terminates in the common penile artery. When sitting and especially when riding a bicycle, a man can cut off blood circulation to this common penile artery. When this artery is damaged, arterial insufficiency and subsequent erectile dysfunction occur. A cavernosal artery supplies blood into each of the erectile bodies of the penis.The blood supply to the glans, or head, of the penis is part of a separate system. It is for this reason that men can achieve an erection without swollen glans, such as in conditions known as priapism.
The underlying mechanism of an erection is the corporo-veno-occlusive mechanism. When the veins cannot become compressed or blocked, an erection cannot be maintained. Without this very sensitive mechanism, blood leaks prematurely from the penis and produces the loss of an erection. This type of erectile dysfunction is called a venous leak.
Nervous System
The nervous system of the penis is involved with both the creation and maintenance of an erection as well as an ejaculation. The most numerous sensory nerves are located on the head, or glans, of the penis. To achieve an erection it takes multiple input from numerous areas of both the brain and the spinal cord. The first part of a
penile erection is controlled by the brain, known as a psychogenic erection. This occurs under any type of mental or erotic stimulation. Penile erections can also be caused by friction of the skin of the penis alone. This is known as a reflexogenic erection, which commonly occurs among men who have had damage to the spinal cord and who are unable to get an erection unless physically stimulated.
Sperm
The scrotum is a unique structure with very thin, loose skin that is slightly hair bearing. It is also controlled by the endocrine system and functions as a receptacle for the testes. Keeping the testicles outside the body produces a cooler environment and thus provides the best area for the creation of sperm to take place. Warmth tends to prevent sperm from developing properly. Underlying the skin of the scrotum is the cremasteric muscle. This muscle is incorporated into the scrotum and by contracting, it elevates the testicles. This is done in response to cool and warm weather and noxious or painful stimuli.The testicles are roughly the size of a small egg. They are responsible for the development of sperm as well as the manufacture of the hormone testosterone. Behind the testicles sits the epididymis, a single coiled tube that is the site of sperm maturation and storage. The end of the epididymis results in a thick muscular tube, called the vas deferens, which carries sperm from the epididymis to the prostate to be ejaculated. The vas deferens is the most common site of sterility operations, or vasectomy. The sperm is carried in the vas deferens to two structures that sit behind the prostate. These structures are called the seminal vesicles, glands roughly 2 inches in length that form a secretion which nourishes the sperm and which attach to the prostate as well. The prostate sits at the base of the bladder and creates a fluid that allows the nourishment and activation of sperm. The primary purpose of both the seminal vesicles and the prostate is to provide nourishment and a place for sperm to live before ejaculation. In fact, the majority of the ejaculate is composed of fluid from both these glands. A very small component, usually less than 5 percent, is actually spermatozoa, which is why the amount of ejaculate remains relatively unchanged after a vasectomy. The prostate secretes the majority of the fluid. Two small glands sit just outside the diaphragm of the urogenital diaphragm, or the thick area that anchors the penis to the pubic bone. These structures, called the bulbourethral glands, produce a very small amount of clear fluid. This is the clear fluid that we see just prior to ejaculation. It may also
contain very small amounts of spermatozoa as well.
Copyright 1998 NTC/Contemporary Publishing Group. From The Impotence Sourcebook, by arrangement with The RGA Publishing Group.
Penis Anatomy and Glossary
The penis contains three major chambers which fill with blood during an erection. These are the Corpora Cavernosa, of which the penis contains two, and the Corpus Spongiosum.
As the expansion of these chambers puts pressure on the tunica albuginea and the blood is trapped in the corpora cavernosa, the penis becomes erect.
The corpus spongiosum also fills with blood, but to a lesser extent than the corpora cavernosa. This is to protect the fragile tissues of the urethra, and permit ejaculation.
The capacity of the corpora cavernosa is the important factor that determines the size of an erect penis. The penis can only become as large as the chambers can allow for, as the erection is dependant on the size of these when fully dilated.
Most penis enlargement methods other than surgery aim to increase the capacity of these chambers, to allow more blood into the penis during erection.
Corona: The 'crown,' a ridge of flesh demarcating where the head of the penis and the shaft join.
Corpa Cavernosa: The corpora cavernosa are the two spongy bodies of erectile tissue on either side of the penis which become engorged with blood from arteries in the penis, thus causing erection.
Corpus Spongiosum: The spongy tissue surrounding the urethra. This tissue expends to protect the urethra when filled with blood, but to a lesser extent than the corpora cavernosa.
Cowper's Glands: The Cowper's glands secrete a small amount of pre-ejaculate fluid prior to orgasm. This fluid neutralizes the acidity within the urethra itself.
Dorsal Side: The top or upper side of the penis.
Ejaculatory Ducts: The path through the seminal glands which semen travels during ejaculation.
Epididymis: The epididymis is a 'holding pen' where sperm produced by the seminiferous tubules mature. The sperm wait here until ejaculation or nocturnal emission.
Foreskin, Prepuce: A roll of skin which covers the head of the penis in uncircumsized men.
Frenulum, Frenum: A thin strip of flesh on the underside of the penis that connects the shaft to the head.
Glans: The glans is visible in the illustration as the head of the penis. The glans in uncircumcised men is usually covered by the prepuce. The glans is highly sensitive, as is the corona, the ridge of flesh that connects the glans to the shaft of the penis.
Head: Also known as the glans, this is the bulbous tip of the penis.
Meatus: The opening at the tip of the penis to allow the passage of both urine and semen.
Perineum: The area between the scrotum and anus.
Prostate Gland: Produces a fluid that makes up the semen. The prostate gland also squeezes shut the urethral duct to the bladder, thus preventing urine from mixing with the semen and disturbing the pH balance required by sperm.
Pubococcygeus Muscle: Also known as the PC or pelvic floor muscle, necessary to control urination and ejaculation.
Raphe: Visible ridge running from the meatus to the perineum across the scrotum, formed during fetus development and gender assignation.
Scrotum: The scrotum is a sac that hangs behind and below the penis, and contains the testes, the male sexual glands. The scrotum's primary function is to maintain the testes at approximately 34 C, the temperature at which the testes most effectively produce sperm.
Semen: Fluid produced during ejaculation, made up of 2-5% sperm. The main bulk of semen is seminal plasma, with large concentrations of Zinc, and amines that protect the sperm from the acidic environment of the vagina.
Seminal Vesicles: The seminal vesicles produce semen, a fluid that activates and protects the sperm after it has left the penis during ejaculation.
Shaft: The main length of the penis made up of the corpora cavernosa, corpus spongisum, urethra, cavernosal artery and dorsal vein and artery.
Smegma: A substance with the texture of cheese made up from oils secreted by glands on each side of the frenulum, combined with skin cells, and moisture. This usually only occurs in uncircumcised men.
Testes, testicles: The male sexual glands, the two testes within the scrotum produce sperm and testosterone. Within each testis is a kilometer of ducts called the seminiferous tubules, the organs which generate sperm. Each testicle produces nearly 150 million sperm every 24 hours.
Urethra: Passageway of the penis, carrying urine from the bladder and semen from the testes to the tip of the penis.
Vas Deferens: The ducts leading from the epididymis to the seminal vesicles. These are the ducts that are cut during the procedure known as vasectomy.
Ventral Side: The bottom, or underside of the penis.
PENIS SIZE
Here are the statistics on erect penis lengths by The Alfred C. Kinsey Institute for Sex Research (from the point where the penis meets the body along the top to its tip):
The average penis length is 6.16 inches. The average girth is 4.84 inches.
 How does erection occur?
How does erection occur?
Erection begins with sexual stimulation. Sexual stimulation can be tactile (for example, by touching the penis), or mental (for example, by having sexual fantasies). Sexual stimulation generates electrical impulses along the nerves going to the penis and causes the nerves to release nitric oxide, which in turn increases the production of cyclic GMP (cGMP) in the smooth muscle cells of the corpora cavernosa. The cGMP causes the smooth muscles of the corpora cavernosa to relax, and allow rapid blood flow into the penis. The in-coming blood fills the corpora cavernosa, making the penis expand.
How is erection sustained?
The pressure from the expanding penis compresses the veins (blood vessels that drain the blood out of the penis) in the tunica albuginea, helping to trap the blood in the corpora cavernosa, thereby sustaining erection. Erection is reversed when cGMP levels in the corpora cavernosa fall, causing the smooth muscles of the corpora cavernosa to contract, stopping the inflow of blood and opening veins that drain blood away from the penis. The levels of the cGMP in the corpora cavernosa fall because it is destroyed by an enzyme called phosphodiesterase type 5 (PDE5)
What is erectile dysfunction?
Erectile dysfunction (ED), also known as impotence, is the inability to achieve or sustain an erection for satisfactory sexual activity. Erectile dysfunction is different from other conditions that interfere with sexual intercourse, such as lack of sexual desire and problems with ejaculation and orgasm. This article focuses on the evaluation and treatment of erectile dysfunction.
How common is erectile dysfunction?
Erectile dysfunction (ED, impotence) varies in severity; some men have a total inability to achieve an erection, others have an inconsistent ability to achieve an erection, and still others can sustain only brief erections. The variations in severity of erectile dysfunction make estimating its frequency difficult. Many men also are reluctant to discuss erectile dysfunction with their doctors, and thus the condition is under-diagnosed. Nevertheless, experts have estimated that erectile dysfunction affects 30 million men in the Untied States.
While erectile dysfunction can occur at any age, it is uncommon among young men and more common in the elderly. By age 45, most men have experienced erectile dysfunction at least some of the time. According to the Massachusetts Male Aging Study, complete impotence increases from 5% among men 40 years of age to 15% among men 70 years and older. Population studies conducted in the Netherlands found that some degree of erectile dysfunction occurred in 20% of men between ages 50 to 54, and in 50% of men between ages 70 to 78. In 1999, the National Ambulatory Medical Care Survey counted 1,520,000 doctor-office visits for erectile dysfunction.

